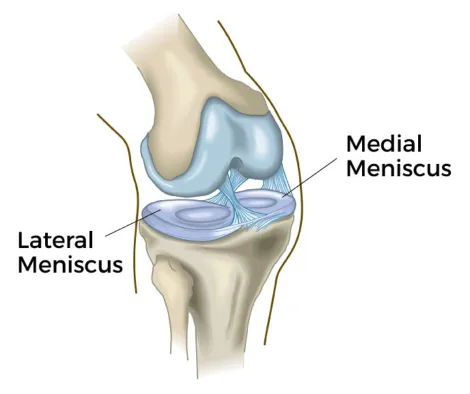
Soft tissue injuries (muscles, ligaments and tendons), are inevitable events during the career of almost every athlete. These injuries usually occur following an impact force from an external stimulus, when there is a contact-related history, or due to strain and/or compression load in the non-contact cases. Most of the non-contact injuries are related with doing too much too fast, after doing too little for too long.
Over the past decades, R.I.C.E.
was the main approach to the management of acute soft tissue injuries, but its effectiveness is being questioned by researchers.
This article provides enriched updated recommendations for optimum and efficient acute soft tissue injury management (from rest & recovery phase to progress to exercise and return to performance), based on a recently published review of research.

All injuries at their initial stage, have to undergo a healing process which is vital to enhance tissue remodeling & recovery. According to the recent data, soft tissue injuries on their immediate care simply need P.E.A.C.E. The acronym arises from
Protection over the first days of an injury is required to minimize bleeding, prevent distension of injured fibers and reduce the risk of injury aggravation by unloading the injured limb and restricting movements that would increase pain.
Elevation while resting (positioning the limb higher than the heart), promotes interstitial fluid flow out of the injured area.
Despite the lack of evidence of its use, elevation is still considered safe given its low risk-benefit ratio. Avoid anti-inflammatory medication (NSAID’s) and ice use over the first 48h as it may potentially disrupt the inflammation process and lead to impaired tissue regeneration in the long-term tissue healing.
As the various phases of inflammation contribute to optimal soft tissue regeneration, inhibiting such an important process using medication or ice is not recommended. When appropriate, NSAID’S dosage should always be prescribed by a licensed health care professional.
Compression (external mechanical pressure) on the injured area, with the use of taping methods, limits intra-articular edema & tissue hemorrhage.
Compression also improves quality of life in ankle sprain injuries. Patient information and education is a major contributing factor and should always be provided by a specialized health professional on these topics in order to raise realistic expectations on the rehabilitation times. Instead of looking for a magic treatment approach up on “Dr” Google, you should consult your physician or physiotherapist to learn more about the nature of your injury condition, recovery times, and how to apply load management.
You should first worry about complete healing and then about the rest & recovery management, as these are key ingredients in any training program. If you don’t allow your body the time needed to recover properly, and instead you push it into exercise the injury won’t heal, while it is also likely to turn into an overuse/chronic condition with persistent symptoms.
Chronic pain is a much greater threat to your sports performance than resting! In general, it's feasible to rest/protect against an injury while still maintaining fitness with modified exercise even from the first days.
How much rest is required prior to exercise introduction, is in general determined by the pain presence and the nature of the injury.
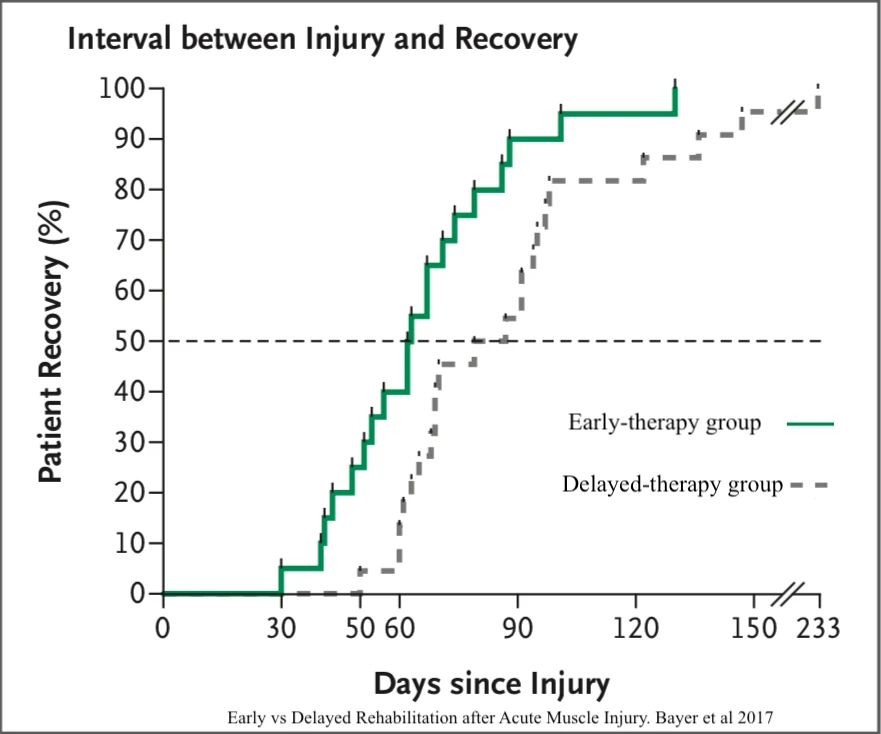
In a recent study, a group of athletes with muscle injuries, who were introduced to exercise sooner (2 days post-injury), shortened the interval from injury to pain-free recovery and returned to sports 3 weeks earlier compared to the athletes who rested for 9 days (see figure). No increased risk of injury recurrence was identified between the two groups. Most of the references set at least a 48h rest period for muscle strains.
When the acute symptoms subside and there is no aggravation in specific movements, pain behavior is guiding the removal of protection and gradual reloading. At this stage, rehabilitation must be driven by L.O.V.E. where the acronym consists of
Optimal loading during the subacute phase of recovery promotes the long-term tissue repair and remodeling, and the capacity of tendons, muscles, and ligaments. Optimal load, as well as persistent pain management for athletes, has been described in another article.
The mental status of the athlete has a key role in sports injury rehabilitation, as emotional distress can decrease significantly the recovery rate. A successful rehabilitation should be driven by consistency, optimism, and trust between the coach, the athlete, and the sports physiotherapist.
A pain-free aerobic exercise represents a cornerstone in the management of musculoskeletal injuries as it boosts athlete’s motivation while at the same time it increases blood flow and facilitates vascularisation to the injured structures. It has also been highlighted that it improves function, work status, optimism while reducing the need for painkillers. Cardiovascular activity is recommended to be introduced as soon as possible, although there are no guidelines on dosage.
In a conclusion, systematic exercise restores mobility, strength, endurance proprioception, agility, and other important aspects of fitness capability, in order to return to desired sports performance. Progression in any activity is been guided by symptoms behavior and comprehensive design.
Any implementation of the provided information should be individualized to fit the biopsychosocial profile of each athlete.
Sources: