Persistent pain in sports performance. Α daily nightmare? “Hurt doesn’t equal harm” is a common mindset, among people who exercise on a regular basis either for recreational purposes or elite sports performance. Phrases like “no pain no gain” or “the pain you feel today is the strength you feel tomorrow” are printed on fitness T-shirts […]

School bags as a cause of back pain. Myth or reality? Back pain is among the most common musculoskeletal conditions of our time, with a continuous increase in incidence rates in the general population, and with frequent reference to age groups among children and adolescents. Epidemiological studies over the world in these age groups have […]

Should I rest or should I load?How to recover following an acute soft tissue injury Soft tissue injuries (muscles, ligaments and tendons), are inevitable events during the career of almost every athlete. These injuries usually occur following an impact force from an external stimulus, when there is a contact-related history, or due to strain and/or […]

When a headache or a toothache is not about the head or teeth? By Zacharias Sifakis & Marios Papachristopoulos Following a stressful day, many people suffer from a telltale pain that radiates from their neck and head and is only preceded by an ongoing stiffness in the jaw. Pain from the temporomandibular joint (TMJ) can […]

Disc herniation is one of the most commonly asked-about subjects and one that there is a lot of misinformation on. We know that: This is a vicious and unnecessary cycle that physios need to educate the public on. 1. What is a disc herniation? A herniated disc in the spine is a condition during which […]
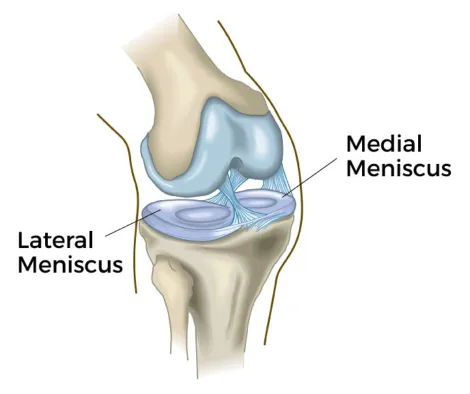
The meniscus is two C-shaped pieces of fibrocartilage (with collagen fibers) that act as shock absorbers between your femur and tibia. The meniscus helps to transmit weight from one bone to another and plays an important role in knee stability. (1,2) A meniscal tear can be due to injury or degeneration due to wear and […]

(Picture from: https://onsurity-in.medium.com/creating-the-ideal-fitness-routine-based-on-your-age-c447c9a9e2fa) Being physically active is one of the most important actions that people of all ages can take to improve their health. The evidence about the health benefits of regular physical activity is well established and has shown that everyone gains benefits from exercising: men and women of all races and ethnicities, young […]

What is scoliosis? Scoliosis is a deformity of the backbone (spine). It’s when the spine has a side-to-side curve and rotation. The curve of the spine measures 10 degrees or more. A normal spine appears straight when looked at from behind. But a child or an adult with scoliosis has a spine with an S […]

Discover the benefits of Clinical Pilates What is Pilates? Pilates is a mind-body exercise system designed to improve balance, strength, flexibility, and posture in a safe and enjoyable way. It focuses on controlled movements, combined with breathing and concentration, to develop a strong and balanced body. What is Therapeutic Clinical Pilates? Clinical Pilates is a […]

All information provided in this section comes from the official website of Keiser Corporation. In our clinic, we have the privilege to possess a Keiser Functional Trainer & Rack. Keiser training appliances are low-inertia resistance devices that eliminate collateral damage from shock loading, to joints and connective tissues, and enable athletes with a prescribed resistance […]