Scoliosis: All you need to know in the simplest way
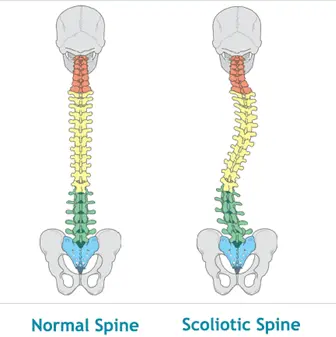
What is scoliosis? Scoliosis is a deformity of the backbone (spine). It’s when the spine has a side-to-side curve and rotation. The curve of the
What is scoliosis? Scoliosis is a deformity of the backbone (spine). It’s when the spine has a side-to-side curve and rotation. The curve of the

(Picture from: https://onsurity-in.medium.com/creating-the-ideal-fitness-routine-based-on-your-age-c447c9a9e2fa) Being physically active is one of the most important actions that people of all ages can take to improve their health. The
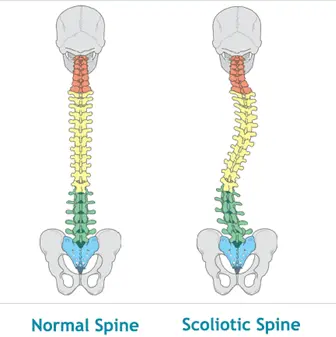
(Picture from: https://blog.crossoversymmetry.com/guide-to-meniscus-tears/ ) The meniscus is two C-shaped pieces of fibrocartilage (with collagen fibers) that act as shock absorbers between your femur and tibia.
Disc herniation is one of the most commonly asked-about subjects and one that there is a lot of misinformation on. We know that: Many people

When a headache or a toothache is not about the head or teeth? By Zacharias Sifakis & Marios Papachristopoulos Following a stressful day, many people

School bags as a cause of back pain. Myth or reality? Back pain is among the most common musculoskeletal conditions of our time, with a
1 Nikiforou Foka
Email: info@chpc.gr
Tel:+30 28210 58711,
+30 6977355112
Kontekaki Street
Email: info@chpc.gr
Tel:+30 28230 43329,
+30 6977355112
Palea EO Chanion Rethimnou
Email: info@chpc.gr
Tel: +30 28250 32807,|
+30 6977355112