When a headache or a toothache is not about the head or teeth?
By Zacharias Sifakis & Marios Papachristopoulos
Following a stressful day, many people suffer from a telltale pain that radiates from their neck and head and is only preceded by an ongoing stiffness in the jaw. Pain from the temporomandibular joint (TMJ) can be easily mistaken for a common headache, mostly because the symptoms are so similar. It often causes for repeated dentist visits without any outcome however as the symptoms arise from a different structure even if you feel it around your teeth.
But there are a few key differences that set a TMJ-related headache or facial pain apart from a common tension headache. When the symptoms are associated with TMJ then the pain state is also known as a temporomandibular disorder (TMD). TMD is a broad term that encompasses disorders of the TMJ and its associated anatomical structures. A TMD can often be very painful and disabling. With an accurate and opportune identification of the type of pain you’re experiencing, you can find relief before the sensation becomes unbearable. But let us have an insight into what we know about one of the joints that we use more on our body.
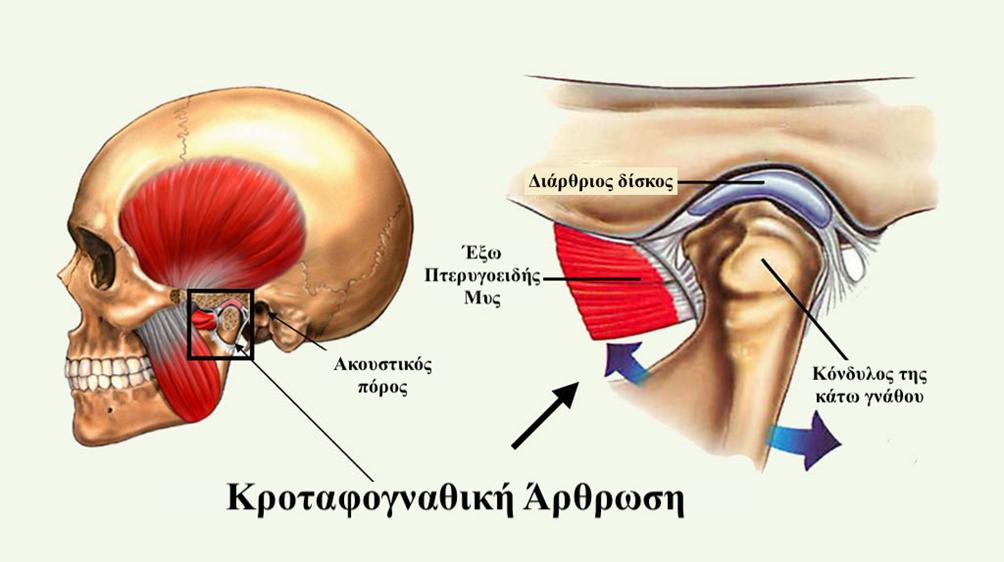
The TMJs are complex structures made up of two bones, the temporal bone and condyle, which are separated by a fibrous disk, and surrounded by a capsule. The TMJ is mainly composed of fibers like those in ordinary connective tissue. This gives the joint the tendency to remodel. Injury to or disorders of these structures can all result in pain in the jaw area. Jaw pain may occur on one side or on both sides, depending upon the cause and may be associated with myofascial pain and headache.
A typical TMD consists of:
• Recurrent pain in one or more regions of the head and/or face.
• X-ray, MRI and/or bone scintigraphy findings that demonstrate TMJ disorder.
Important clinical evidence that pain can be attributed to the TMD are:
– Pain precipitated by jaw movements such as laughing, yawning and/or chewing of hard or tough food.
– Jaw stiffness and reduced range of motion or irregular jaw opening.
– Noises like clicking or popping) from one or both TMJs during jaw movements.
– Tenderness of the joint capsule(s) in one or both TMJs.
Temporomandibular disorders may occur following a direct trauma or secondary due to indirect mechanism of injury. Usually, direct trauma is a blow or a fall to the chin or jaw. Indirect mechanisms of injury may be triggered by numerous causes. Most common are whiplash injury following an accident, heavy chewing, teeth grinding (bruxism), clenching of the jaw, disorders of dental occlusion, loss of dental height due to worn down or missing teeth, prolonged periods of mouth opening such as a dental or a general anaesthetic procedure etc.
Common intra-articular temporomandibular disorders are inflammation, internal derangement conditions, and degeneration. These conditions are commonly related to a disk/condyle incoordination and noise can be detected on movements. This may progress to locking (where the condyle can’t ride over the forward located disk) where the mouth can not open causing symptoms and severe limitations in daily activities such as chewing, laughing or yawning. Overuse of the jaw muscles such as excessive gum chewing can inflame the TMJ, resulting in pain and stiffness.
Arthritis can also occur in the TMJ as a result of age-related degeneration (usually seen in the over 50s), or secondary to trauma occurring at a younger age. In arthritis, crepitus can be felt or heard and changes can often be seen on a plain x-ray or on an MRI.
Muscle spasm of one or more muscles of mastication, is an extra-articular cause of TMD usually following prolonged dental procedures or anaesthetics or due to stress, bruxism etc. Muscle spam can also cause significant pain and limitation of the jaw movements. Mismanagement of fractures rehabilitation, at the mandibular symphysis or the condylar neck, as well as the dislocation of one or both condyles, can also be a cause for a TMD.
It is not always clear what triggers a TMD and there are numerous other conditions that can cause pain in the TMJ region. Pain in the areas of the face around the TMJ’s, jaws and ears, often derives from common disorders of the upper cervical spine.
Specialised clinical examination, as well as an interdisciplinary approach where needed, is required to ensure a reliable differential diagnosis & treatment is given, and that potentially serious problems such as trigeminal neuralgia, systemic diseases and other medical conditions are not overlooked.
What is the treatment and prognosis for temporomandibular disorders?
TMD is a recurring, but self-limiting condition that tends not to be progressive and usually responds to conservative therapy. TMJ-related pain is commonly misdiagnosed as a regular stress-induced headache. TMJ-related pain in fact is a much more preventable source. Following successful treatment, headache resolves within 3 months and does not recur.
Satisfactory management requires a thorough clinical examination. The examination should include complete history of the patient, assessment of jaw/tongue/neck position, palpation of the TMJ, assessment of both active and passive range and quality of movement of the jaw and cervical spine, and assessment of the patient’s bite. Also, signs of sleep bruxism/grinding are checked. Important clinical signs including the presence of swelling, muscle spasm and stiffness or hypermobility of one or both TMJ. Complaints of limited mouth opening and other signs of joint dysfunction must also be interpreted and assessed in the context of age, gender, and general health.
Α personalised identification of the factors contributing to a TMD, can be decisive in establishing the most effective therapy. In some of the cases, a simple modification of lifestyle and oral habits may be sufficient to alter symptom intensity. Non-invasive, conservative treatments include physical therapy, occlusal adjustment, splint therapy (especially when symptoms are related to bruxism during sleep), medications etc.
Given the self-limiting nature of most TMD, surgical intervention is rarely the treatment of choice, but may be justified in cases where circumstances are extreme, and disability associated with joint disease impacts greatly on the quality of life.
Physiotherapy treatment is an effective and safe approach in the treatment and management of TMD, even when the symptoms are long-standing and severe. With the appropriate comprehensive approach, most patients will see a significant improvement in pain intensity and range of motion within 3 to 6 weeks. Individualized accustomed mobility exercise programmes and selection of manual therapy techniques have the most promising effects in people with TMD.
This article is intended to promote understanding of and knowledge about a common health topic and does not intend to be a substitute for professional advice, diagnosis or treatment. As the evidence cannot determine the most appropriate type, intensity, and duration of therapy, we recommend you to always seek the advice of your dentist, specialized physiotherapist or other qualified healthcare providers with any questions you may have regarding a medical condition or treatment on the TMJ area.
Sources:
• https://physio-pedia.com/Temporomandibular_Disorders#sts=Other%20Causes%20of%20TMJ%20and%20Facial%20Pain
• https://www.sciencedirect.com/science/article/abs/pii/S1532338217302956?via%3Dihub
• https://www.medicinenet.com/temporomandibular_joint_syndrome_tmj/article.htm
• https://americanmigrainefoundation.org/resource-library/temporomandibular-disorders-and-headache/
• https://www.healthline.com/health/tmj-headache#causes
• https://www.sciencedaily.com/releases/2006/05/060514082537.htm?_ga=2.121202568.1427160655.1564678119-848101992.1564678119
• https://www.colgate.com/en-us/oral-health/conditions/temporomandibular-disorder/tmj-headache-1115
• https://journals.sagepub.com/doi/abs/10.1177/0269215516672275?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=crea
• https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4706597/
• https://www.ncbi.nlm.nih.gov/pubmed/17185065
• https://www.nhs.uk/conditions/trigeminal-neuralgia/causes/
• https://www.nhs.uk/conditions/trigeminal-neuralgia/causes/